If you have been diagnosed with endometrial hyperplasia, you might be feeling worried or confused about what it means for your health.
Endometrial hyperplasia is a condition where the lining of the uterus (the endometrium) becomes thicker than normal.
This can cause abnormal bleeding, such as heavy periods, spotting between periods, or bleeding after menopause.
Endometrial hyperplasia is not cancer, but in some cases, it can develop into cancer if left untreated.
The good news is that most cases of endometrial hyperplasia can be treated effectively and safely with medication or surgery.
In this blog post, I will explain what causes endometrial hyperplasia, how it is diagnosed, and what are treatment options available.
What causes Endometrial Hyperplasia?
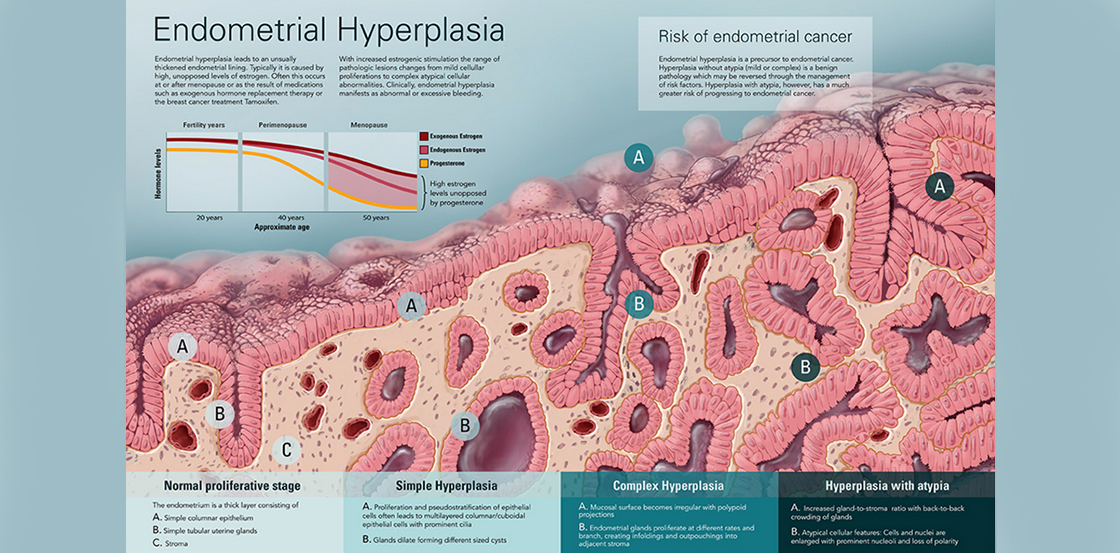
The main cause of endometrial hyperplasia is an imbalance of hormones in the body.
Hormones are chemical messengers that regulate many functions in the body, including the menstrual cycle.
The two main hormones that affect the endometrium are oestrogen and progesterone. Oestrogen stimulates the growth of the endometrium, while progesterone keeps it in check.
Normally, the levels of oestrogen and progesterone change throughout the menstrual cycle, resulting in a regular shedding of the endometrium as a period. However, sometimes the balance of these hormones can be disrupted, leading to too much oestrogen and not enough progesterone.
This can cause the endometrium to grow too thick and not shed properly.
Some factors that can increase the risk of developing endometrial hyperplasia are:
- Being overweight or obese
- Having polycystic ovary syndrome (PCOS)
- Taking hormone replacement therapy that has unbalanced HRT (e.g. Sequential HRT)
- Having irregular or absent periods
- Being close to menopause or postmenopausal
How is Endometrial Hyperplasia diagnosed?
The usual case scenario is a woman has had abnormal bleeding and undergoes an ultrasound scan or gynaecology scan where there is suspicion of endometrial hyperplasia… and
A typical ultrasound report could be something like….
The most common test in the UK when endometrial hyperplasia is suspected is, the offer of hysteroscopy and endometrial biopsy, which involves looking inside the womb with a telescope (hysteroscopy) taking a small sample of tissue from the lining of the uterus (Endometrial biopsy) and examining the biopsy sample under a microscope.
This will achieve two things,
- Hysteroscopic assessment of the womb cavity gives the professional an opportunity to assess the lining of the womb in its entirety and can take a directed biopsy and rule out the existence of other pathologies such as polyp or sinister pathology which can sometimes be missed on ultrasound.
- A biopsy could be a random sampling of the lining of the womb or a directed biopsy which the specialist thinks is the most appropriate area to sample.
This can show if there is any abnormality in the cells of the endometrium.
There are different types of endometrial hyperplasia, depending on how abnormal the cells look and how likely they are to turn into cancer.
The types are:
- Simple hyperplasia without atypia: This is the most common and least serious type of endometrial hyperplasia. The cells are slightly enlarged and irregular, but not very different from normal cells. The risk of developing cancer from this type is less than 5% over 20 years.
- Complex hyperplasia without atypia: This type involves more cells than normal and they are more crowded and irregular. The risk of developing cancer from this type is about 10% over 20 years.
- Simple hyperplasia with atypia: This type involves enlarged and irregular cells that also have abnormal features called atypia. Atypia means that the cells look more like cancer cells than normal cells. The risk of developing cancer from this type is about 25% over 20 years.
- Complex hyperplasia with atypia: This is the most serious type of endometrial hyperplasia. It involves many abnormal cells that are crowded and irregular and have atypia. The risk of developing cancer from this type is about 50% over 20 years.
Treatment Options
The treatment for endometrial hyperplasia depends on several factors, such as:
- The type and severity of the condition (e.g. Simple hyperplasia, complex hyperplasia, presence of atypia or not)
- Your age and whether you want to have children in the future
- Your symptoms and preferences
- Your general health and medical history (e.g. Having weight issues such as obesity)
The main goal of treatment is to restore the normal balance of hormones in the body and prevent the endometrium from growing too thick or becoming cancerous.
The treatment options include:
- Observation: This means monitoring your condition with regular check-ups and biopsies to see if it improves on its own or gets worse. This option may be suitable for women who have simple hyperplasia without atypia, especially if they have reversible risk factors such as obesity or HRT use that can be addressed. However, you should be aware that observation alone has a lower success rate than medication or surgery, and you may still need treatment later if your condition does not improve or worsens.
- Medication: This involves taking pills or using an intrauterine device (IUD) that contains a hormone called progestin. Progestin is a synthetic form of progesterone that can counteract the effects of estrogen and shrink the endometrium. This option may be suitable for women who have any type of endometrial hyperplasia, especially if they want to preserve their fertility or avoid surgery. However, you should be aware that medication may have some side effects such as weight gain, mood changes, or breast tenderness, and you may still need surgery later if your condition does not improve or worsens.
- Surgery: This involves removing the uterus (hysterectomy) and sometimes the ovaries (oophorectomy) as well. This option may be suitable for women who have complex hyperplasia with atypia, who have failed to respond to medication or observation, who have persistent bleeding or pain, or who do not want to have children in the future. However, you should be aware that surgery is a major procedure that has some risks and complications such as infection, bleeding, or damage to nearby organs, and it will also stop your periods and make you unable to get pregnant.
The duration of treatment and follow-up for endometrial hyperplasia varies depending on the type of treatment and the outcome.
Generally, medication should be taken for at least 6 months to see if it works and then continued for longer if it does.
Surgery should be followed by regular check-ups to make sure there is no recurrence of the condition or development of cancer. In any case, you should always consult your doctor before starting or stopping any treatment, and report any changes in your symptoms or health.
What can you do to prevent Endometrial Hyperplasia?
While you cannot control all the factors that may cause endometrial hyperplasia, there are some things you can do to reduce your risk and improve your health.
These include:
- Maintaining a healthy weight: Being overweight or obese can increase the levels of oestrogen in your body and make your endometrium thicker. Losing weight can help restore the balance of hormones and prevent abnormal bleeding.
- Eating a balanced diet: To consider reduced intake of foods of animal origin
- Exercising regularly: Physical activity can help you burn calories, lower your blood pressure, improve your mood, and reduce stress. It can also help regulate your menstrual cycle and balance your hormones.
- Limiting alcohol intake: Drinking too much alcohol can increase the levels of oestrogen in your body and make your endometrium thicker. It can also damage your liver and impair its ability to break down hormones.
- Using contraception: If you are sexually active and do not want to get pregnant, you should use a reliable form of birth control that suits your needs and preferences. Some forms of contraception, such as combined oral contraceptives or progestin-only pills or IUDs, can also help prevent endometrial hyperplasia by regulating your hormones and thinning your endometrium.
- Taking HRT with caution: If you are menopausal or perimenopausal and need hormone replacement therapy (HRT) to relieve your symptoms, you should talk to your doctor about the benefits and risks of different types of HRT. You should avoid taking HRT which contains only estrogen, as this can increase the risk of endometrial hyperplasia and cancer. You should also take the lowest dose possible for the shortest time possible and have regular check-ups and biopsies to monitor your condition.
Conclusion
Endometrial hyperplasia is a common condition that affects many women at some point in their lives. It is not cancer, but it has the potential to lead to cancer if left untreated.
The treatment options for endometrial hyperplasia depend on several factors, such as the type and severity of the condition, your age and fertility plans, your symptoms and preferences, and your general health and medical history.
The main goal of treatment is to restore the normal balance of hormones in the body and prevent the endometrium from growing too thick or becoming cancerous. The treatment options include observation, medication, or surgery. The duration of treatment and follow-up for endometrial hyperplasia varies depending on the type of treatment and the outcome.
You can also take some steps to prevent endometrial hyperplasia by maintaining a healthy weight, eating a balanced diet, exercising regularly, quitting smoking, limiting alcohol intake, using contraception, and taking HRT with caution.
If you have any questions or concerns about endometrial hyperplasia or its treatment, please do not hesitate to contact us and clear your concerns. We are here to support you and provide you with the best care possible. Remember that you are not alone in this journey, and we are always happy to hear from you