Post link copied to clipboard!
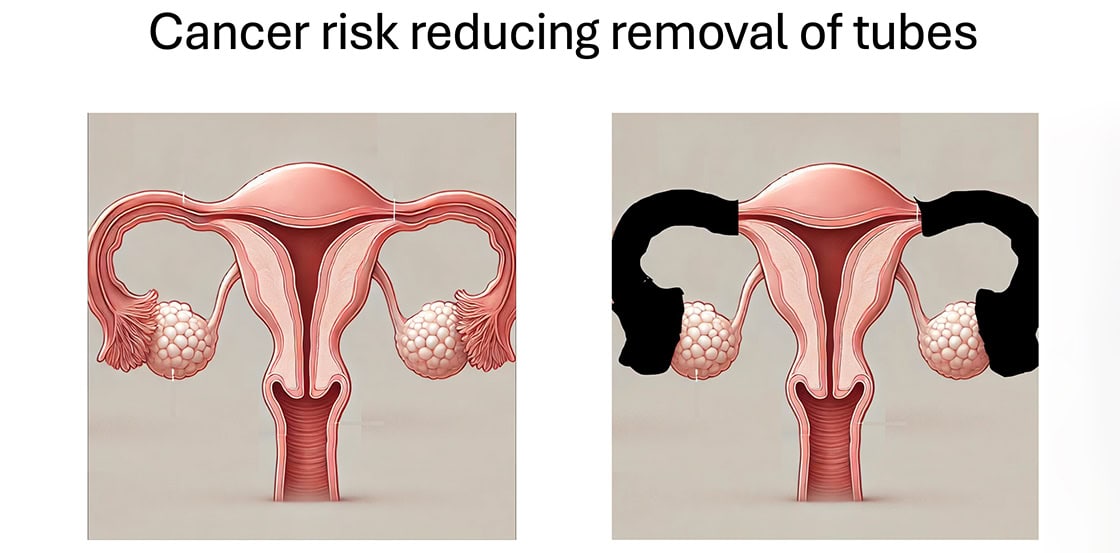
Ovarian cancer is a serious health issue, often diagnosed late because there’s no effective screening test. It has been discovered that most high-grade ovarian cancers likely to start in the fallopian tubes. This finding has led to new preventive strategies, such as risk-reducing salpingectomy (RRS) or removal of tubes or removal of Fallopian tubes, which involves removing the fallopian tubes while keeping the ovaries.
For many women, especially those with a high risk of ovarian cancer (like BRCA1 and BRCA2 mutation carriers), traditional preventive measures involve removing both the ovaries and fallopian tubes (RRSO). While this can greatly reduce cancer risk, it also induces early menopause, leading to symptoms like hot flushes and increasing the risk of heart disease and osteoporosis. Removal of tubes offers a promising alternative by potentially preventing cancer without these severe side effects.
Research has shown that high-grade serous carcinomas often originate in the fallopian tubes. By removing these tubes, we could reduce the chances of developing ovarian cancer, even in women who don’t carry specific genetic mutations but have other risk factors.
Several studies have looked into whether removing the fallopian tubes affects ovarian function. The findings are reassuring: there appears to be no significant impact on hormone levels or ovarian health. Moreover, the procedure doesn’t add much risk during surgeries like hysterectomy or sterilisation.
Experts are increasingly recommending salpingectomy for women undergoing surgery for other benign reasons, like hysterectomy, or those seeking sterilisation. This “opportunistic salpingectomy” is becoming a common practice because it can significantly reduce cancer risk without additional health risks.
Women with a high risk of ovarian cancer, such as those with BRCA mutations, traditionally undergo RRSO by age 40. However, there’s growing interest in “interval salpingectomy with delayed oophorectomy” (ISDO), where the tubes are removed first, delaying ovary removal to reduce menopause-related side effects. This approach could be particularly beneficial for younger women not ready for the consequences of early menopause.
Ongoing research aims to confirm the benefits and safety of these procedures, especially ISDO. Trials like the Women Choosing Surgical Prevention (WISP) trial are crucial for understanding how these surgeries affect the quality of life and cancer risk.
Risk-reducing salpingectomy represents a significant step forward in ovarian cancer prevention. As more evidence supports its safety and effectiveness, it’s becoming a standard option for many women. This approach has the potential to save lives and to preserve the quality of life by preventing the onset of early menopause and its associated risks. As medical knowledge and practices evolve, women have more options than ever to manage their cancer risk proactively.